Manual platelet counting is a traditional method for determining platelet concentration in blood samples, ensuring accuracy in clinical diagnostics and research applications․
1․1 Importance of Manual Platelet Counting
Manual platelet counting is crucial for accurate platelet concentration determination, especially in cases with low platelet levels or when automated methods fail․ It ensures precise results, offering a reliable alternative for clinical and research purposes, and is cost-effective for small-scale or specialized analyses․
1․2 Brief Overview of Platelet Counting Methods
Platelet counting methods include manual and automated techniques․ Manual counting uses a hemocytometer for precise platelet enumeration, while automated analyzers provide high-throughput results․ Blood smear estimation offers a quick assessment․ Each method serves distinct purposes, with manual counting being cost-effective for small-scale analyses and automated methods suited for rapid, large-scale testing in clinical settings․

Materials and Equipment Required
Essential materials include a hemocytometer, microscope, pipettes, and diluting fluids for accurate manual platelet counting and sample preparation․
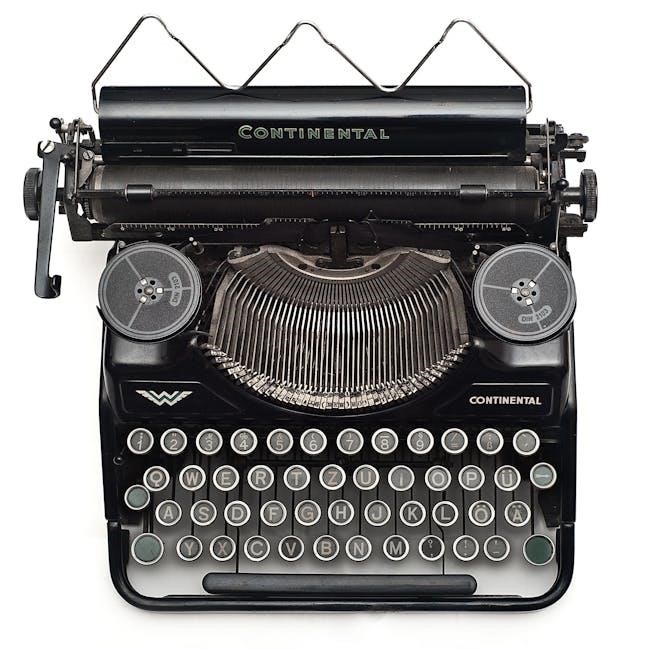
2․1 Hemocytometer (Counting Chamber)
A hemocytometer is a specialized glass chamber used for counting cells and platelets under a microscope․ It features a precise grid etched into its surface, allowing for accurate enumeration of particles within specific volumes․ The chamber is designed to hold a measured sample, ensuring consistency and reproducibility in manual counting methods․ Proper calibration and handling are essential for reliable results․
2․2 Microscope and Accessories
A microscope with adjustable magnification (typically 100x and 400x) is essential for manual platelet counting․ It requires a built-in stage, focus knobs, and a condenser for optimal illumination․ Accessories like immersion oil enhance clarity, while a reticle or grid helps in counting within specific fields․ Proper maintenance and calibration ensure accurate visualization and enumeration of platelets in the hemocytometer․
2․3 Diluting Fluids and Pipettes
Diluting fluids, such as 1% ammonium oxalate or formaldehyde, are used to prevent clotting and maintain platelet stability․ Accurate pipettes, including manual and automated options, ensure precise measurement of blood and diluent volumes․ These tools are critical for achieving the correct dilution ratio, enabling accurate platelet enumeration in the hemocytometer․ Proper handling and calibration of pipettes are essential for reliable results․
Blood Sample Preparation
Blood samples are collected using phlebotomy techniques and anticoagulants like EDTA to prevent clotting․ Proper mixing ensures uniform platelet distribution, crucial for accurate manual counting procedures․
3․1 Collecting and Handling Blood Samples
Blood samples for manual platelet counting are typically collected using phlebotomy techniques with anticoagulants like EDTA to prevent clotting․ Proper mixing of the sample ensures uniform platelet distribution․ Handling requires careful avoidance of hemolysis or contamination․ Samples should be stored at room temperature and processed within a few hours to maintain platelet viability for accurate counting․
3․2 Dilution Process for Manual Counting
The dilution process involves mixing blood samples with a diluent, such as ammonium oxalate, to reduce viscosity and prevent platelet clumping․ A typical ratio is 1:100, ensuring accurate counting under a microscope․ Proper mixing and precise measurement are critical to avoid errors․ This step standardizes the sample, enabling reliable platelet enumeration in the hemocytometer․
Counting Technique
Manual platelet counting involves using a microscope and a hemocytometer to systematically count platelets in specific fields, ensuring accurate and reliable results for clinical assessment․
4․1 Loading the Hemocytometer
Properly loading the hemocytometer is critical for accurate platelet counting․ Place the chamber on the microscope stage, draw diluted blood into a pipette, and allow the sample to fill the chamber via capillary action․ Ensure no air bubbles form and the sample spreads evenly across the counting grid․ This step ensures precise platelet distribution for accurate manual counting․
4․2 Counting Platelets in the Microscope
Under the microscope, locate the counting chamber’s grid, focusing on the 25 large squares․ Count platelets in each corner square, noting those touching the middle lines․ Average counts from multiple fields, adjusting for dilution․ Multiply by 10,000 to estimate platelets per microliter․ Ensure accurate focus and lighting for clear visibility, avoiding air bubbles and clumps for reliable results․

Platelet Count Formula
The formula calculates platelets per microliter: (average count per 25 squares × 10,000) ÷ dilution factor․ For example, 100 platelets in 25 squares equals 40,000 platelets/µL․
5․1 Step-by-Step Calculation Process
Count platelets in 25 large squares of the hemocytometer․ 2․ Calculate the average count per square․ 3․ Multiply by 10,000 to account for dilution․ 4․ Divide by the dilution factor to determine platelets per microliter․ This systematic approach ensures accurate and reliable results․
5․2 Interpreting the Results
After calculating, compare the platelet count to the normal range of 150,000-450,000 platelets per microliter․ Low counts may indicate thrombocytopenia, while high counts suggest thrombocytosis․ Ensure consistency across multiple fields to validate accuracy․ Document any abnormalities for further clinical assessment․
Normal Platelet Count Range
The normal platelet count ranges from 150,000 to 450,000 platelets per microliter of blood․ Average healthy individuals typically have counts between 200,000 and 400,000 platelets/µL․ This range may vary slightly depending on the laboratory or individual health conditions․
6․1 Average Platelet Count in Healthy Individuals
In healthy individuals, the average platelet count typically ranges from 150,000 to 400,000 platelets per microliter of blood (µL)․ Most people have a count between 200,000 and 300,000/µL․ This range is considered normal and essential for proper blood clotting․ Variations may occur due to age, sex, or other factors, but significant deviations warrant further medical evaluation to rule out underlying conditions․ Accurate measurement is crucial for clinical assessments․
6․2 Factors Affecting Platelet Count
Platelet count can be influenced by various factors, including age, sex, and overall health․ Conditions like infections, inflammation, or bone marrow disorders may cause fluctuations․ Additionally, certain medications, stress, or nutritional deficiencies can impact platelet levels․ Accurate interpretation of platelet counts requires consideration of these variables to ensure reliable and meaningful results in clinical or research settings;
Common Errors in Manual Counting
Common errors include incorrect dilution, improper hemocytometer loading, and miscounting platelets due to overlapping or debris, impacting accuracy and reliability of manual platelet counting results․
7․1 Sources of Inaccuracy
Common sources of inaccuracy in manual platelet counting include incorrect dilution of blood samples, improper loading of the hemocytometer, and inconsistent counting techniques․ Additionally, human error, such as miscounting platelets or failing to account for debris, can lead to inaccurate results․ Proper training and adherence to standardized protocols are essential to minimize these errors and ensure reliable outcomes in manual platelet counting procedures․
7․2 Tips for Improving Accuracy
To enhance accuracy in manual platelet counting, ensure precise dilution of blood samples and consistent chamber loading․ Use standardized counting techniques, and examine multiple fields to minimize variability․ Regularly calibrate equipment and participate in training to maintain proficiency․ Clear documentation and adherence to laboratory protocols further ensure reliable and reproducible results in manual platelet counting procedures․

Comparison with Automated Platelet Count
Manual platelet counting offers reliability for small samples, while automated methods provide faster, high-throughput results with improved accuracy for large-scale testing in clinical settings․
8․1 Advantages and Disadvantages of Manual vs․ Automated Methods
Manual platelet counting is cost-effective and precise for small samples but requires skilled personnel and is time-consuming․ Automated methods are faster and scalable but may lack accuracy in complex samples․ Manual methods are ideal for specialized cases, while automated counting is preferred for high-throughput settings due to efficiency and consistency in results․
Clinical Significance of Platelet Count
Platelet count is crucial for diagnosing bleeding disorders, thrombocytopenia, and thrombocythemia, guiding treatment decisions and assessing bleeding or clotting risks in clinical settings․
9․1 Indications for Platelet Count Testing
Platelet count testing is essential for diagnosing thrombocytopenia, thrombocythemia, and bleeding disorders․ It is also used to monitor conditions like leukemia, HIV, or sepsis, and to assess bleeding risks before surgery or in pregnancy complications․ Additionally, it helps evaluate clotting abnormalities and monitor responses to treatments affecting platelet production․
9․2 Interpreting Abnormal Results
Abnormal platelet counts indicate conditions like thrombocytopenia (low platelets) or thrombocythemia (high platelets)․ Low counts may suggest bleeding risks or diseases like leukemia or HIV, while high counts could indicate myeloproliferative disorders․ Results must be correlated with clinical symptoms and patient history․ Confirmatory tests, such as blood smears, are often required to validate findings and guide appropriate treatment plans․
Advanced Considerations
Advanced techniques involve specialized counting methods, such as adjusting for microscopic field size variations, to enhance accuracy in complex or challenging blood samples․
10․1 Specialized Counting Techniques
Specialized techniques include adjusting for microscopic field size variations and using predefined multiplication factors to enhance accuracy․ These methods are particularly useful in complex samples where platelet clumping or irregular distribution occurs․ Advanced protocols may involve counting multiple fields and calculating averages to ensure reliable results, especially in research or clinical settings requiring precise platelet count determination․
10․2 Troubleshooting in Platelet Counting
Common issues include platelet clumping, uneven distribution, or incorrect dilution, leading to inaccurate counts․ To address these, ensure proper mixing of samples, verify dilution ratios, and count multiple fields for consistency․ Using a standardized hemocytometer and calibrated microscope helps minimize errors․ Regularly cleaning equipment and following precise protocols can also enhance reliability and accuracy in manual platelet counting procedures․
Manual platelet counting remains a reliable method for determining platelet concentration, utilizing a hemocytometer and microscope properly․ Adhering to the formula ensures accurate and consistent results in clinical settings․
11․1 Summary of Key Points
Manual platelet counting involves using a hemocytometer and microscope to accurately determine platelet concentration․ The process includes diluting blood samples, loading the counting chamber, and applying the formula․ The manual count formula multiplies the average platelet count per field by 15,000 to estimate the total platelets per microliter․ This method ensures reliable results when adhering to proper techniques and controls, making it a valuable tool in clinical and research settings․
11․2 Best Practices for Manual Platelet Counting
Adhere to standardized protocols for consistent results․ Ensure proper blood sample handling and accurate dilution․ Use a calibrated hemocytometer and microscope․ Count platelets in multiple fields to minimize variability․ Record counts systematically and apply the correct formula․ Regularly maintain and calibrate equipment․ Train personnel thoroughly to avoid human error․ Use appropriate quality controls to validate results, ensuring reliable and reproducible outcomes․
